南方医科大学南方医院放疗科李娜ASCO现场报道。
2016年6月3日,一年一度的美国临床肿瘤学会(AmericanSocietyofClinicalOncology, ASCO)年会在芝加哥盛大召开。本次大会收录了多个我国学者主导的肿瘤前沿研究。当地时间6月4日上午,南方医科大学南方医院放疗科朱晓霞教授团队进行的可手术切除IIIA-N2期非小细胞肺癌(NSCLC)术后放疗的Meta研究于壁报展出,该研究评估了术后放疗在可手术切除IIIA-N2期NSCLC中的价值。
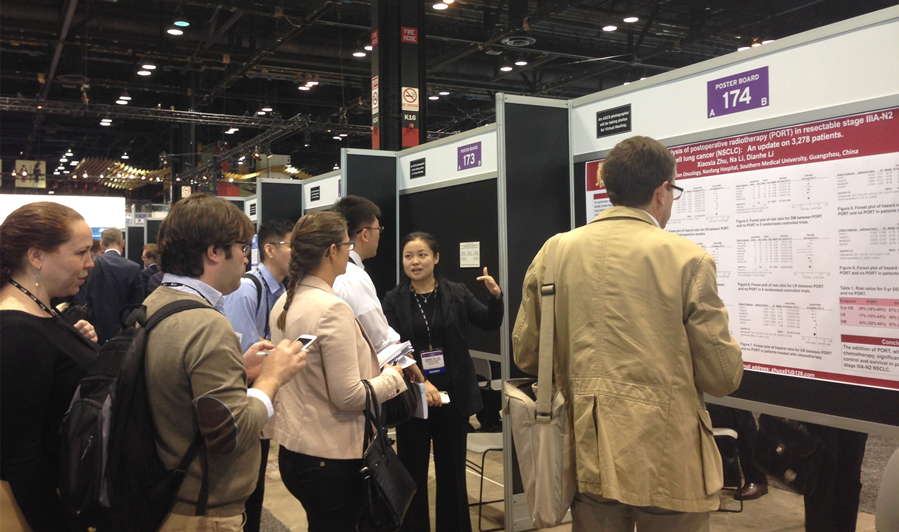
朱晓霞教授与外国专家交流
研究概况
该研究共纳入8个随机对照试验(779例患者)和8个回顾性研究(2499例患者)。
结果分析显示,与单纯手术相比,术后放疗延长了总生存(HR 0.73,95%CI 0.58-0.92,P=0.007)。
5年生存率由接受单纯手术治疗患者中的21%增加到接受术后放疗患者中的29%。
术后放疗也有助于降低局部复发率(RR 0.64,95%CI 0.50-0.82,P<0.001)和远处转移率(RR0.74,95% CI 0.62-0.88,P<0.001),并能改善局部无复发生存(HR 0.37,95% CI 0.24-0.58,P<0.001)和无病生存(HR0.70,95% CI 0.60-0.83,P<0.001)。
亚组分析显示,接受了化疗或采用三维适形放射治疗技术的患者可以从术后放疗获得更多的生存获益,HR分别为0.61(95%CI 0.41-0.91,P=0.02)与0.60(95%CI 0.42-0.85,P<0.004)。
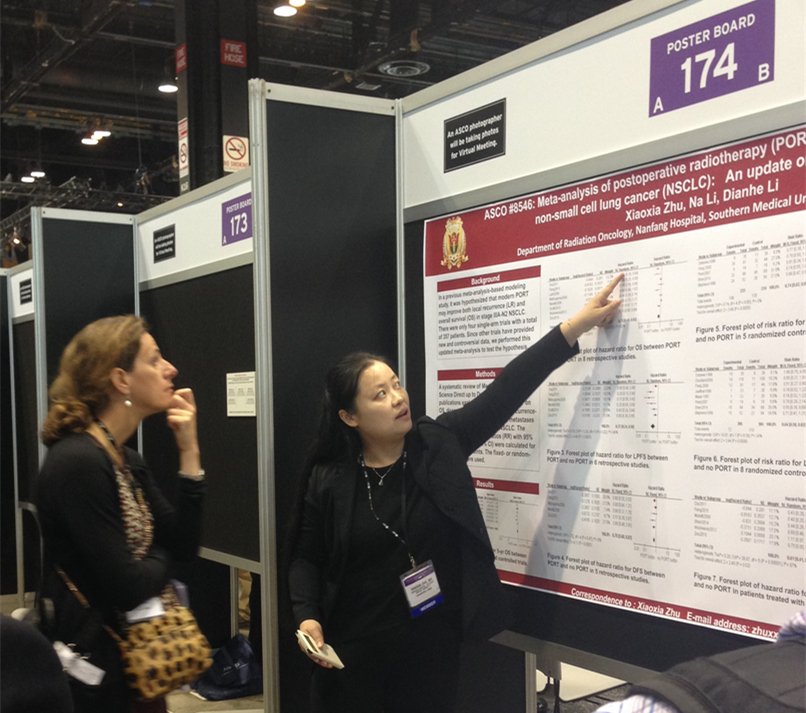
朱晓霞教授为外国专家介绍研究
热点关注
壁报内容受到较多国内外与会者的关注,关注的热点为术后化放疗联合的模式(序贯还是同步)、术后放疗的范围(全纵隔预防还是累及区域预防)、术后放疗的剂量以及N2的状态(单站N2还是多站N2)对研究的结果是否有影响。
朱晓霞教授认为,目前可切除IIIA-N2期NSCLC术后放疗的应用证据基于的多为回顾性研究数据,前瞻性随机对照研究多为单中心、样本量偏小的研究,而且多数研究中采用的放疗技术陈旧、放疗剂量(21-60Gy,1.8-3.0Gy/F)及范围不统一,这些都会降低现有临床证据的效力。
有关上述大家关注的可能影响可手术IIIA-N2期NSCLC术后放疗疗效判读的因素的临床对照研究数据更是缺乏,因此急需开展基于现代精确放疗技术、统一放化疗方案的多中心的前瞻性随机对照研究,为术后放疗在可手术IIIA-N2期NSCLC中的应用提供更高级别的证据和规范,并指导获益人群的选择。
会议专题》》》2016年ASCO年会专题报道
摘要阅读
Abstract No:8546
Meta-analysisof postoperative radiotherapy (PORT) in resectable stage IIIA-N2 non-small celllung cancer (NSCLC): An update on 3,278 patients
Session: Lung Cancer—Non-SmallCell Local-Regional/Small Cell/Other Thoracic Cancers
Type: Poster Session
Author(s): Na Li, Xiaoxia Zhu,Yiyi Li,et al.
Background: In a previous meta-analysis-basedmodeling study, it was hypothesized that modern PORT may improve both localrecurrence (LR) and overall survival (OS) in stage IIIA-N2 NSCLC. There wereonly four single-arm trials with a total of 357 patients. Since other trialshave provided new and controversial data, we performed this updatedmeta-analysis to test the hypothesis.
Methods: A systematic review of Medline, Cochrane andScience Direct up to December 2015 identified publications exploring theefficacy of PORT on OS, disease-free survival (DFS), local recurrence-freesurvival (LRFS), LR, and distant metastases (DM) in resectable stage IIIA-N2NSCLC. The hazard ratios (HR) and risk ratios (RR) with 95% confidenceintervals (95% CI) were calculated for pre-specified endpoints. The fixed- orrandom-effect models were used.
Results: Overall 16 trials comprising 3,278 patientswere included. There was a significant benefit in favor of PORT regarding OS(HR 0.73, 95% CI 0.58-0.92, p = 0.008; absolute benefit at 5 years = 8%), DFS(HR 0.70, 95% CI 0.60-0.83, p < 0.0001), LRFS (HR 0.37, 95% CI 0.24-0.58, P< 0.0001). Restriction of the analysis to trials with induction and/oradjuvant chemotherapy (CT) led to similar results. PORT significantly decreasedthe risk of LR (RR 0.64, 95% CI 0.50-0.82, P = 0.0006) and DM (RR 0.74, 95% CI0.62-0.88, P = 0.0005), and the absolute risk differences were 13% and 14%respectively.
Conclusions: The addition of PORT, with orwithout CT, significantly improves local control and survival in patients withresectable stage IIIA-N2 NSCLC.
打开微信 →→ 添加“医脉通肿瘤科”公众号,或扫描电脑屏幕右上方二维码 →→ 关注医脉通肿瘤科。随时随地获取肿瘤前沿资讯,一次打包最实用的肿瘤治疗知识。做科研达人、临床高手,尽在医脉通肿瘤频道。
