近期J Clin Oncol 上发表的一篇研究,探讨了使用蒽环霉素和紫杉醇治疗早期乳腺癌患者的最佳给药方案。医脉通对此进行了报道。
研究原文:Budd GT,J Clin Oncol 2014 Nov 24
研究方法
该研究采用2×2的析因设计,来检测关于治疗淋巴结阳性或高风险的淋巴结阴性的早期乳腺癌患者的两种不同方案的假设是否正确1.一种新的阿霉素-环磷酰胺的持续方案优于六个周期每两周一次的阿霉素-环磷酰胺。2.每周一次紫杉醇优于六个周期每两周一次的紫杉醇。研究共纳入了3250位患者,每个随机试验的无病生存风险比为0.82,检验效能为90%,双侧α=.05。该研究将总生存作为次要观察结果。
研究结果
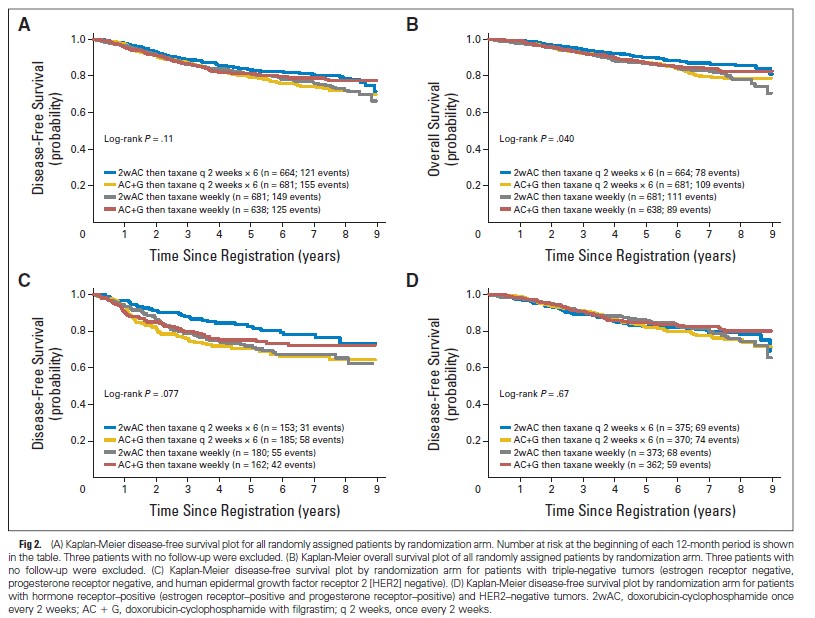
期中分析跨越了无用界限。结果显示每周一次的方案和每2周一次的方案都具有优越性。中位随访时间为6年。在初始试验设计中,随机分配了2716位患者,两个随机因子之间有显著的相关性 (DFS P =_ .024; OS P= _.010),该试验排除了两个因子分别的干预作用。
比较全部4组的结果显示,OS有显著差异(P= _.040),但是DFS没有(P= _ .11)。所有每2周给药一次的治疗都与更高的OS 相关。OS的差异似乎受限于激素受体阴性或人类表皮生长因子受体2(HER2)阴性肿瘤(P= _ .067)。激素受体阳性/HER2阴性(P= _ .90)或HER2阳性的肿瘤没有观察到差异(P= _ .40)。
结论
使用任意一种方案的患者均得到相似的DFS。亚组分析显示每2周一次用药可能是激素受体阴性/HER2阴性肿瘤的最佳方案。
摘要原文:
Purpose
To determine the optimal dose and schedule of anthracycline and taxane administration as adjuvant therapy for early-stage breast cancer.
Patients and Methods
A 2× 2 factorial design was used to test two hypotheses: (1) that a novel continuous schedule of doxorubicin-cyclophosphamide was superior to six cycles of doxorubicin-cyclophosphamide once every 2 weeks and (2) that paclitaxel once per week was superior to six cycles of paclitaxel once every 2 weeks in patients with node-positive or high-risk node-negative early-stage breast cancer. With 3,250 patients, a disease-free survival (DFS) hazard ratio of 0.82 for each randomization could be detected with 90% power with two-sidedα=.05 Overall survival (OS) was a secondary outcome.
Results
Interim analyses crossed the futility boundaries for demonstrating superiority of both once-perweek regimens and once-every-2-weeks regimens. After a median follow-up of 6 years, a significant interaction developed between the two randomization factors (DFS P =.024; OS P= .010) in the 2,716 patients randomly assigned in the original design, which precluded interpretation of the two factors separately. Comparing all four arms showed a significant difference in OS (P = .040) but not in DFS (P= .11), with all treatments given once every 2 weeks associated with the highest OS. This difference in OS seemed confined to patients with hormone receptor–negative/ human epidermal growth factor receptor 2 (HER2) –negative tumors (P= .067), with no differences seen with hormone receptor–positive/HER2-negative (P = .90) or HER2-positive tumors (P =.40).
Conclusion
Patients achieved a similar DFS with any of these regimens. Subset analysis suggests the hypothesis that once-every-2-weeks dosing may be best for patients with hormone receptor– negative/HER2-negative tumors.
